Learn how massage can improve your life

Welcome back to Body Mechanics Study Corner where we do all the research so you don’t have to! Actually, Matt does all the research. Normally he does this to satiate his own thirst for knowledge and drive to learn any findings that could make him a better massage therapist, but once again we are offering up the fruits of his labor up to you all. We hope you find it enlightening and interesting.
“Sleep is the golden chain that ties health and our bodies together” -Thomas Dekker What is sleep hygiene? The CDC defines sleep hygiene as “the good habits that can lead to you getting a good night’s sleep” As a yoga therapist, I talk a lot about sleep hygiene and refer our clients to sleep hygiene […]

Whether it’s another exhausting election cycle or the impending zombie apocalypse, many of us are a bit more stressed and anxious lately than usual. Intense times, it’s totally normal to start experiencing some physical symptoms that might feel abnormal if you don’t realize their source. Some of your old injuries might start hurting again, your […]

Our Massage Therapist, Matt Danziger sits down with the Knowledge Exchange to talk Manual Therapy or, rather what manual therapy is NOT in this blog/podcast One of the things we pride ourselves over here at Body Mechanics Orthopedic Massage is our devotion to science and giving people a real outlook on what massage can and […]

Relax…. You book the massage appointment. You take the risk. It is a financial stretch but you have to do something because you have not been able to manage on your own. You lay down on the table. The massage therapist says “Take a deep breath…Relax…” In the last few years, I have become very […]
Massage Therapy and Pain Working with Clients in the Pain Zone This is a continuation of the last pain blog which offered some history on pain science and also some really general guidelines on massage therapy and pain. If your client has no red flags in assessment and you have decided it is safe to […]
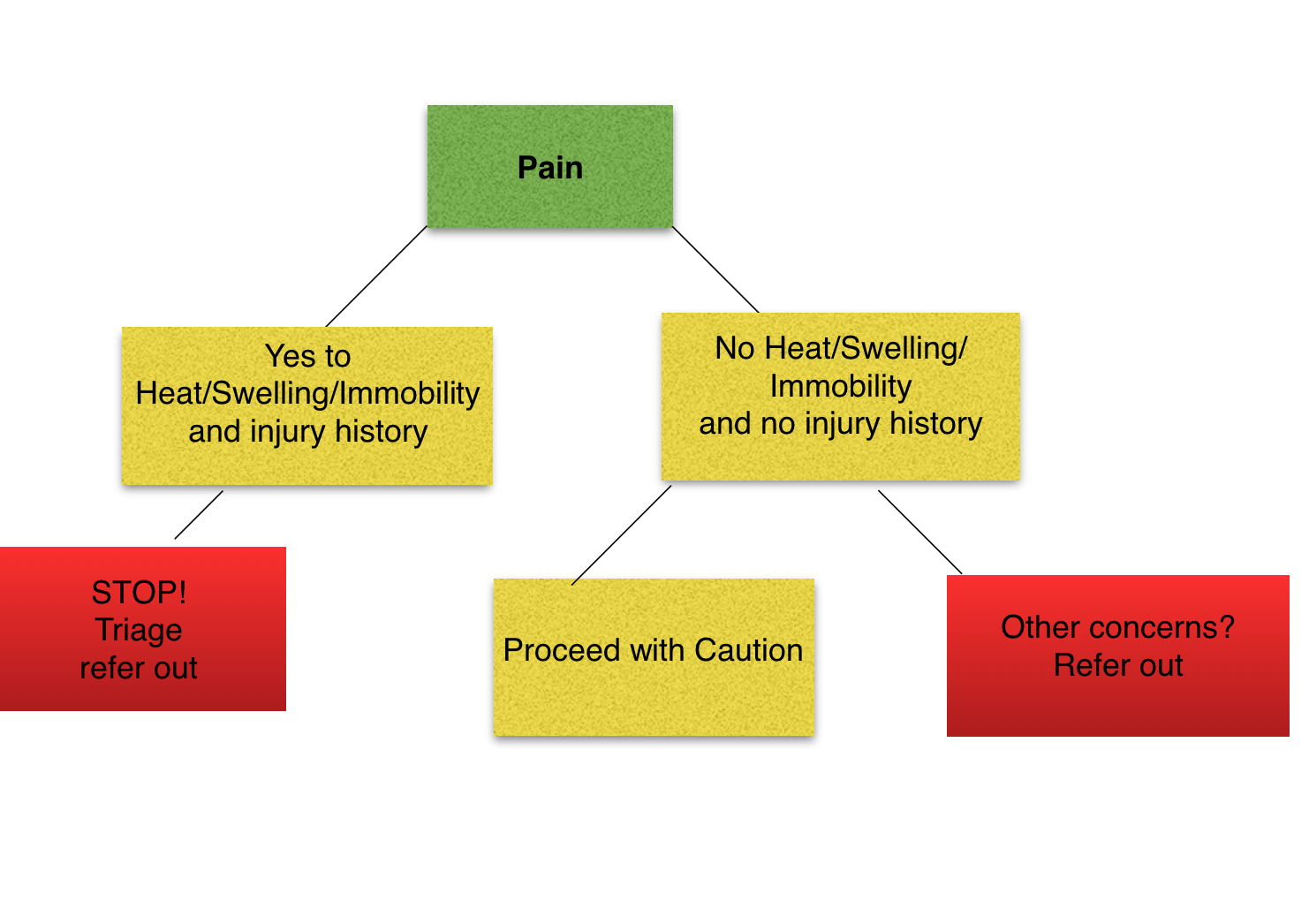
Massage therapists live in a world of touch. So it is no surprise that the new science that relates to how touch, sensation and pain is processed and experienced would be relevant to massage therapists. This is particularly true since many clients seek out massage therapy for complaints specifically relating to pain. Pain science in […]