Learn how massage can improve your life
This blog was inspired by the fact that we spend a lot of time trending hard and obsessing over modalities. We debate whether they are ‘right’ or ‘wrong’ and what we as therapists should be doing now. Recently I talked with a very aggressive young therapist who was willing to alienate many of his current […]

How do you know you know what you know? Massage Mythology Let’s examine massage mythology. As therapists, every time we perform our techniques, we also engage in a variety of other ritualistic and protocol-oriented tasks. For example, the client comes into the space, they lay down on the table, you dim the lights, you […]
Massage therapy and Science Based Massage Well after being so serious I just could not take it any more and this happened. At my clinic we are science based, we are all well educated massage professionals who believe in massage therapy as a science rather than as a fantasy of our own making. In […]
Massage Therapy and Pain Working with Clients in the Pain Zone This is a continuation of the last pain blog which offered some history on pain science and also some really general guidelines on massage therapy and pain. If your client has no red flags in assessment and you have decided it is safe to […]
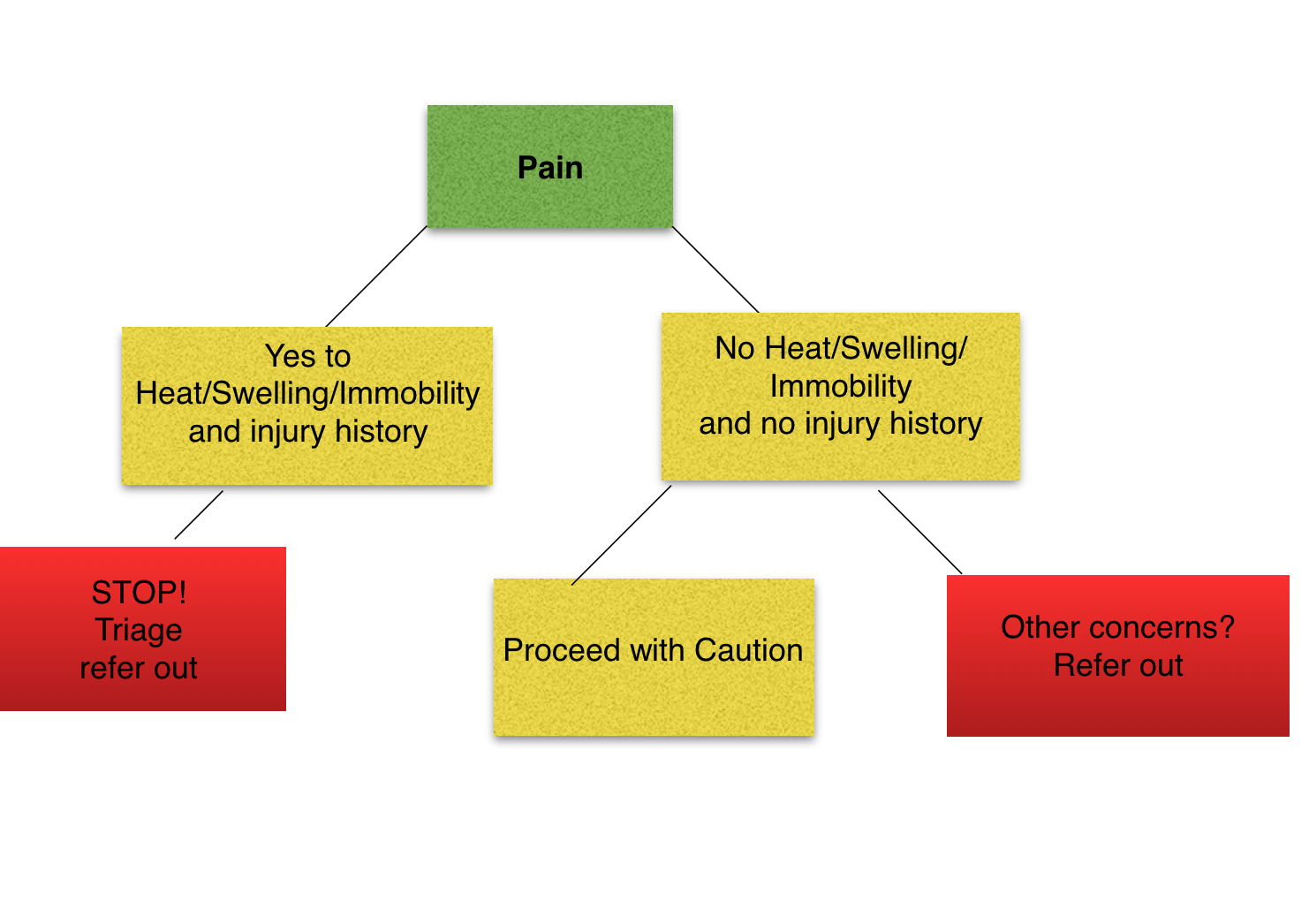
Massage therapists live in a world of touch. So it is no surprise that the new science that relates to how touch, sensation and pain is processed and experienced would be relevant to massage therapists. This is particularly true since many clients seek out massage therapy for complaints specifically relating to pain. Pain science in […]
What the heck are we doing with Orthopedic Massage? So this post is inspired by my frustration at some of the myths that perpetrate the massage industry through poor education, misinformation, poor training and subsequently are passed on to the general public. Orthopedic Massage is a science-based practice based largely on evidence. While our understanding […]

By Ivan Garay LMT/CPT Strength training can improve a cyclist’s performance and protect against injuries. Research on endurance athletes shows that strength training improves the three most important predictors of endurance sports performance[1]: economy (the ability to do a certain amount of work using as small amount of energy as possible), velocity/power at maximal […]

The right strengthening and stretching program is important when preparing for a marathon. Strength training has been shown to improve running economy, prevent injuries, and improve body composition and resting metabolic rates. Strength training is particularly important for older runners. Endurance exercise, like running, does less to protect against age related loss of lean muscle […]
Exercises for Plantar Fasciitis Plantar Fasciitis is one of the most common foot complaints. Technically what is happening is the plantar fascia is being over stretched or over taxed Beret Kirkeby, “Treating Plantar Fasciitis” Exercise for plantar fasciitis should reduce excessive strain on the plantar fascia and correct biomechanical faults that contribute to plantar fasciitis. […]
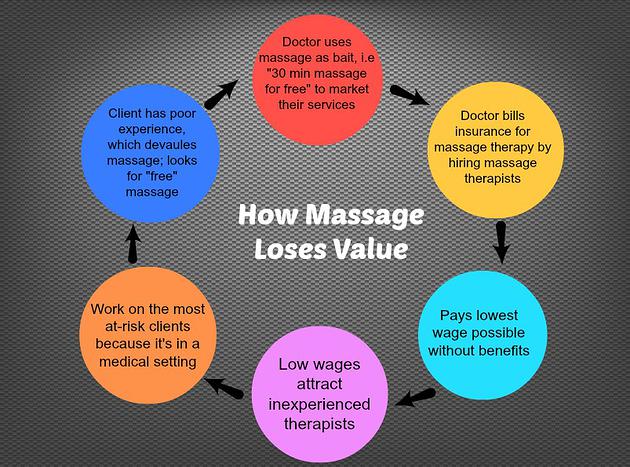
This is a brief description on how massage loses its value in the wrong hands. We encourage you to find independent therapists, small companies, or health professionals who do the manual work themselves, to break the cycle.